2. 43 Abbreviation: PrEP, pre-exposure prophylaxis. Table 6. Female Sex Workers: Synopsis of Problem and Desired Behaviours and Practices PROBLEM BEHAVIOURS/PRACTICES DESIRED BEHAVIOURS/PRACTICES • Inconsistent use of prevention methods • Larger number and rapid exchange of partners • Transient nature looking for more clients; some sex workers move around to hot spots, e.g. tobacco auctions, mines or trucking routes; some will leave for weeks at a time to go with a trucking client • Insufficient privacy and inconsistent schedule for taking HIV treatment • Exposure to violence; disempowered to insist on use of condoms • Does not seek preventive services; lack of (awareness and) access to sex worker-friendly health care services • Fear in disclosing HIV-positive results to clients • Fear around attending local clinic for HIV testing due to lack of provider confidentiality; financial barrier to seek services further away with an unknown provider • Misuse of drugs or alcohol • Reduce risky behaviours that increase risk of HIV infection • Increase awareness and understanding of risk (especially for women negotiating transactional sex who might not consider themselves a sex worker) • Seek/use HIV prevention (testing, self-testing, male and female condoms, lubricants and PrEP), care and treatment products and services • Identify supportive environments to ensure adequate social support; reduce stigma • Seek HIV testing, including HIV self-testing for themselves and partners • Empower sex workers with knowing their human rights • Advocate for safe sex • Providers to deliver empathetic, female-friendly and confidential care • Increase awareness of income-generation programs and projects • Improve knowledge of HIV risk among clients of sex workers; modified attitudes and perceptions about risk; use of prevention methods during interactions
1. 42 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Female Sex Workers FSW: Situation and Behavioural Analysis HIV prevalence among female sex workers in Zimbabwe is 57.1%, which is nearly five times the rate of the general population. 8 There are an estimated 4,000 new HIV infections among FSWs annually. 35 In Zimbabwe, 30% of men aged 30-49 and 25% of married men and 19% of men with secondary or more education reported having sex with a commercial sex worker. 33 Sex workers and their clients are at high risk of HIV due to the large number and rapid change of sexual partners, high rates of STIs, dry sex and sex during menses. 34 Other contributing factors include unsafe working conditions and violence (by law enforcement officials, intimate partners and clients), the inability to negotiate condom use, social stigma and discrimination and criminalised work environments. 35 Public and private humiliation are significant challenges for sex workers that prevent them from seeking health care services and support from their communities. 36 The HIV care cascade for FSWs is lagging behind the general population as only 64% of those living with HIV know their status, 68% of those who know their status are currently on treatment and 77% of those on treatment are virally suppressed. More needs to be done to ensure that FSWs are tested and linked to prevention and treatment services and are supported to adhere to treatment. 37 Financial Barriers Research on sex work has shown that the price of sex without a condom can be four times the price of sex with a condom. 34 Often sex workers fear losing a client if they insist on sex with a condom. Other financial limitations are access to condoms and medications. Often sex workers do not have enough condoms to match the number of clients. Moreover, despite antiretrovirals (ARVs) being provided for free, the transport costs and user fees (e.g. council clinics) required are enough to make the medications unaffordable and inaccessible. Due to economic conditions and the lack of employment opportunities, 34 many women feel stuck in sex work even if they would like to have the opportunity for other forms of work. Health Care Services Many sex workers use local clinics in emergencies only—they prefer clinics specific for sex workers as they feel more understood. In general clinics, sex workers fear stigma and do not feel comfortable disclosing their profession. Data report that less than half of FSWs diagnosed with HIV went for referral assessment and ART initiation and that only 14% attended more than one appointment. 36
6. 47 * For simplicity, all content within this matrix matches the HIV status and journey of the archetype. However, a desired change along with matching illustrative messages have been identified for the alternative HIV status. Abbreviations: ART, antiretroviral therapy; IEC, information, education and communications; PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis; STI, sexually transmitted infection. Illustrative Messages • I always carry my medication with me so I do not miss a dose • I adhere to my medication to stay healthy • Keep the viral load low—stay healthy and maintain the good looks • Being adherent to your medications and using condoms consistently and correctly keeps you healthy, and prevents reinfection • No condom, no sex • Use lubricant to prevent condom breakages. • Don’t compromise, condomise • It is my right to negotiate for safe sex—I use condoms • Stay in control, use condoms to prevent STIs and unplanned pregnancy • I am an empowered woman—I use a condom always • Use family planning services to protect yourself from unplanned pregnancies • Children by choice, not by chance • My health, my responsibility Illustrative Messages for desired change for HIV negative: To maintain negative HIV status through prevention methods (PrEP, condoms, STIs, PEP)* • Taking care of my health is my business—I am using PrEP • My health and my future are in my hands—I take PrEP medicines daily • PrEP helps me to be in control of my health/life • I understand my risk—I take PrEP • No condom, no sex • Lubricants help to prevent condom breakages • It is my right to negotiate for safe sex—I use condoms • Don’t compromise, condomise • Stay in control—use condoms • Prevent STIs—use condoms • Worried about sexual violence? Ask about PEP • If you have been a victim of sexual violence, using PEP within 72 hours can reduce risk of contracting HIV Illustrative Indicators 1. % of target audience expressing accepting attitudes to female sex workers accessing HIV and sexual reproductive health services 2. Percentage increase in female sex worker satisfaction with provider services 3. % of target audience with accurate knowledge of (a) HTS, (b) HIV prevention, (c) care and treatment, (d) viral load testing, (e) how ART alters disease, (f) HIV medication side effect management and (g) family planning methods side effect management 4. % of female sex workers who report knowledge of where to access (a) HIV testing, (b) HIV prevention, (c) care and treatment, (d) viral load testing services and (e) family planning methods and services 5. % of female sex workers who can recall the risk of HIV re-infection and STIs 6. % of female sex workers who report that they know how to use condoms consistently and correctlyy 7. % of female sex workers who agree that condoms provide effective protection against (a) unintended pregnancy, (b) STIs, (c) HIV and (d) all 8. Number of female sex workers accessing family planning methods
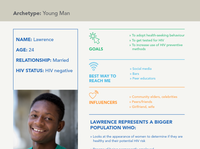
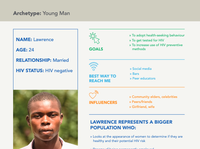
3. 44 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 “I want to use condoms with my clients, but they will pay me more money not to. Even when I tell them I’m HIV positive, they don’t believe me because I look healthy” Archetype: Female Sex Worker » Queens » Clients » Peers » SMS, WhatsApp » Sex worker Queens, peers » Peer educators Abbreviations: ARV, antiretroviral; STI, sexually transmitted infection. » To achieve viral load suppression » To use condoms consistently and correctly » To prevent unplanned pregnancy NAME: Tsitsi AGE: 24 RELATIONSHIP: Has children and a long-term boyfriend HIV STATUS: HIV positive GOALS BEST WAY TO REACH ME INFLUENCERS TSITSI REPRESENTS A BIGGER POPULATION WHO : » Has clients who prefer not to use condoms and will pay her more money for sex without one; her boyfriend also doesn’t want to use condoms » Travels to clients (tobacco farmers, truck drivers, miners) » Describes health as staying free of illness and looking healthy and having beautiful skin » Feels she can talk about health with her peers and at sex worker clinics » Is more worried about earning money than having safe sex » Can’t get her ARVs refilled when she’s away from her health facility » Doesn’t know her rights as a patient and has a low level of self-efficacy when seeking services; she keeps her work a secret from her family » Seeks services far away from her home so that the provider won’t know her » Tells the health care worker that she is married to explain that her husband gave her the STI » Gets a lot of information from peer educators (especially when they come to her work environments such as bars, sex worker ‘Queen’ and via WhatsApp group texts; she also spends time at church) » Thinks HIV self-testing is a good way to test her long-term boyfriend Female Sex Worker Health Journey Map: Tsitsi, 24 years old, HIV positive About this map: This is a theoretical high-level health journey for a female sex worker interacting with HIV and SRH programmes, which may overlap or be sequential. The journey map reveals her experience and what she might be doing, thinking and feeling along the way that impact her desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Sex worker ‘Queens’, WhatsApp groups, peer educators, health workers at sex worker clinics; Other sources: radio and TV, peers Limited Opportunities: When her husband found out she had HIV, he divorced her and kicked her out. She turned to sex work to support her children. Though she is motivated to stay healthy for her children, she often can not afford the fees associated with transport and ARVs, and also feed her children. She wants to find other work, but employment opportunities are limited Financial Barriers: Worrying about money triggers unsafe behaviour because men pay more money for condomless sex. Staying sober helps her have more power to negotiate condom use, though sometimes when she discloses her HIV status, client s do not believe her and still do not want to use a condom. Women’s empowerment and access to high-quality condoms combined with education and awareness for men about HIV risk factors are helpful strategies to encourage condom use Privacy and Confidentiality: Client confidentiality, privacy and provider stigma, in addition to costs (time away from other needs and financial expenses like transport and fees) prevent her from seeking services from health clinics. She does not want to get pregnant as it will impede her ability to work
5. 46 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Communications Matrix: Female Sex Workers DESIRED CHANGES* TO ACHIEVE VIRAL SUPPRESSION TO USE CONDOMS CORRECTLY AND CONSISTENTLY TO PREVENT UNINTENDED PREGNANCY Barriers • Provider and community stigma towards sex workers • Self-stigma • Client privacy and confidentiality • Low knowledge of viral load (what it is, where to get tested and benefits of suppression) • Side effects from medications (feel dizzy, sick, etc.) • High mobility; transient and inconsistent schedule • Lack of privacy to take medications • Long turnaround for viral load results • Clients refuse to use condoms • Clients pay more money for not using condoms • Clients do not perceive risk because sex worker looks healthy • Perceived difficulty using male and female condoms • Lack of knowledge of appropriate and available family planning methods • Side effects of family planning methods (bleeding, weight gain) Facilitating Factors • Desire to be healthy to support children • Viral load testing availability • All public health facilities provide ART • Desire to stay healthy • Sex worker queen’s endorsement • Peer influence • Availability and accessibility of male and female condoms • Availability of family planning IEC material • Low cost of family planning methods • Wide availability of family planning and counselling services in public, private and specialised (sex worker) facilities Communications Objectives 1. Reduce self-directed stigma and health worker stigma and discrimination 2. Increase knowledge, attitudes and perceptions on the importance of viral load testing and disease progression, including how ART alters disease progression 3. Increase knowledge, attitudes and perceptions of ART side effects 4. Increase knowledge of where to access ART medications 5. Increase knowledge of risk of HIV reinfection and STIs 6. Increase knowledge on benefits of consistent and correct use of male and female condoms 7. Increase self-efficacy to negotiate for condom use 8. Increase knowledge, attitudes and perceptions of appropriate and available modern family planning methods
4. 45 Female Sex Worker Health Journey Map: Tsitsi, 24 years old, HIV positive About this map: This is a theoretical high-level health journey for a female sex worker interacting with HIV and SRH programmes, which may overlap or be sequential. The journey map reveals her experience and what she might be doing, thinking and feeling along the way that impact her desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Sex worker ‘Queens’, WhatsApp groups, peer educators, health workers at sex worker clinics; Other sources: radio and TV, peers Limited Opportunities: When her husband found out she had HIV, he divorced her and kicked her out. She turned to sex work to support her children. Though she is motivated to stay healthy for her children, she often can not afford the fees associated with transport and ARVs, and also feed her children. She wants to find other work, but employment opportunities are limited Financial Barriers: Worrying about money triggers unsafe behaviour because men pay more money for condomless sex. Staying sober helps her have more power to negotiate condom use, though sometimes when she discloses her HIV status, client s do not believe her and still do not want to use a condom. Women’s empowerment and access to high-quality condoms combined with education and awareness for men about HIV risk factors are helpful strategies to encourage condom use Privacy and Confidentiality: Client confidentiality, privacy and provider stigma, in addition to costs (time away from other needs and financial expenses like transport and fees) prevent her from seeking services from health clinics. She does not want to get pregnant as it will impede her ability to work Positive emotion Neutral emotion Negative emotion Tsitsi’s Experience Key Insights Doing: Fixes her hair, goes to work Thinking: I wish there were other job opportunities so I could leave sex work Feeling: Frustrated, Ambivalent, Resolved Doing: Gets ready for work, fixes herself up Thinking: “No condom, no sex” that’s my moto; I do not want to get re-infected with another strain of HIV Feeling: Empowered, Optimistic, Proud Doing: Takes the bus to pick up HIV medications at the health facility Thinking: I can not afford the clinic user fees or transport fees to collect my ARVs Feeling: Worried Doing: Goes to work at the bar from 6pm to 6am Thinking: I need to stay sober so that I can negotiate safe sex Feeling: Determined, Nervous Doing: Travels to hot spots to find more clients Thinking: It’s hard for me to take my ARVs regularly because of my erratic schedule and I share a room when I travel, but I want to stay healthy Feeling: Defeated, Lost, Worried Doing: Has unprotected sex with a client Thinking: I hope I do not get pregnant; but I needed the extra money and he paid more to have sex without a condom Feeling: Angry, Stressed, Frustrated Doing: Goes to the clinic for a pregnancy test. Thinking: I need to get on birth control pills, but I am worried that the provider will know my HIV status and tell other people Feeling: Worried, Self- Protective, Frustrated, Lost, Ashamed Doing: Talks to the provider at sex worker clinic and discusses birth control methods; learns about the female condoms Thinking: I am glad to learn more about the female condoms; I wonder if there are additional options Feeling: Empowered, Relieved, Educated Care and Treatment Prevention: Condoms Family Planning Abbreviations: ART, antiretroviral therapy; ARV, antiretroviral; FSW, female sex worker; SRH, sexual and reproductive health.