6. 69 * For simplicity, all content within this matrix matches the HIV status and journey of the archetype. However, a desired change along with matching illustrative messages have been identified for the alternative HIV status. Abbreviations: ART, antiretroviral therapy; PrEP, pre-exposure prophylaxis. Illustrative Messages • Take care of your health – use family planning services, get tested for HIV and protect yourself • I care about my family. I want to know my status • In my social circle, we talk about HIV testing • My HIV status does not affect my relationship with God • My partner and I choose when to have a baby— all of my children are planned • Children by choice, not by chance • Protect yourself - know your status, take PrEP and prevent other STI infections • I take care of my health—I use PrEP • Taking care of my health is my business—I am using PrEP • I learnt how to manage the side effects—now I feel great • My health and my future are in my hands—I take PrEP medicines daily • I am not afraid of being in control. I use PrEP • I am PrEP’ed • I understand my risk—now I take PrEP • My health is my responsibility, so I take PrEP • Break the silence of HIV. Begin by talking with your partner • Know your partner’s status, protect yourself • I talked to my partner about HIV and we went together to get tested • It was not easy to talk to my partner about HIV, but we saw a counsellor together and developed a shared understanding • My partner is my best friend. We talk about everything, including our HIV status Illustrative Messages for sub-desired change for HIV positive: To get initiated on ART and stay virally suppressed* • Being HIV positive is not the end of the world—take your medica tion to stay alive and healthy • My family is supportive so taking my medication is easy • I have HIV and it is undetectable because I take my medication • I found a support group to help me stay on treatment—I feel better • Now I understand why taking my HIV medication is so important —I can live a long, healthy and normal life • I take my HIV medications to keep my viral load low—that reduces the risk of transmission to my partner • It is in the best interest of my family to stay health, so I am on ART • I take my medication, so I can stay healthy and see my grandchildr en grow Illustrative Indicators 1. % of community members who report positive perceptions of women accessing family planning methods 2. % of clients satisfied with provider attitude when delivering health services 3. % of providers who report positive attitudes for women accessing HIV services 4. % of adult women who can recall benefits of HIV prevention methods including PrEP 5. # of providers trained on identifying and screening at-risk populations 6. % of adult women who report having talked to their partner about the benefits of couples counselling and testing 7. # of partners of adult women who report having heard of messages about couples counselling and testing
2. 65 Abbreviations: ANC, antenatal care; GBV, gender-based violence; IPV, intimate partner violence; PMTCT, prevention of mother-to-child transmission of HIV; PrEP, pre-exposure prophylaxis; SRH, sexual and reproductive health; VMMC, voluntary medical male circumcision. Table 9. Adult Women: Synopsis of Problem and Desired Behaviours and Practices PROBLEM BEHAVIOURS/PRACTICES DESIRED BEHAVIOURS/PRACTICES • Does not seek HIV, family planning or pregnancy services • Unfavorable attitudes and perceptions and limited knowledge among pregnant and lactating women and community members about (the benefits of) ANC/PMTCT, 46 SRH and HIV prevention methods (HIV testing/self-testing, male and female condoms, VMMC, PrEP) • Socio-cultural and religious beliefs inhibit use of modern health services • Has unprotected sex with her husband; low HIV risk perception • Does not/cannot negotiate safe sex; powerlessness/lack of empowerment to negotiate safer sex and condom use 45 ; low condom use among married couples • Husbands do not want to get tested for HIV; low rate of partner testing 45 • Fear of GBV/IPV for disclosing HIV negative or positive results to partner or family 46 • Poor adherence to medications; gap between knowledge and practice of adhering to medication; lack of disclosure; insufficient social support; financial barriers • Improve awareness, knowledge, perceptions, attitudes and use of HIV prevention (self-testing, male and female condoms, and PrEP), care and treatment • Use of SRH services to prevent unintended pregnancy and promote the need for ANC/PMTCT • Seek community supports to enhance self-efficacy to access HIV prevention, care and treatment services • Negotiate and practice safer sex • Providers to deliver empathetic, female-friendly and confidential care • Seek safe and secure HIV couples counselling and testing • To go for ANC visits and HIV testing
1. 64 COMPREHENSIVE NATIONAL HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Adult Women AW: Situation and Behavioural Analysis HIV prevalence among women continues to increase between ages 25-29 (14.3%) and 30-34 (22%) and peaks between ages 40-44 (29.6%). 7 Adult women at highest risk of HIV infection include those in serodiscordant relationships or with a partner of unknown status, and pregnant and lactating women due to unsafe sexual practices; gender-based and intimate partner violence (GBV and IPV); social, cultural and gender norms. Low condom use among married couples and sexual networks—including husbands who have young girlfriends or visit sex workers—contribute to the increased risk of HIV infection among adult women. Gender-Based and Intimate Partner Violence GBV and IPV—including physical, sexual or psychological harm or suffering—is a violation of basic human rights and a key driver of the HIV epidemic. Women ages 25-29 experience the highest rate (42.4%) of ever experiencing physical violence (since age 15); moreover, 13% to 16% of women ages 25-49 have ever experienced sexual violence. 33 Substance abuse (such as high levels of alcohol consumption) and determinants such as husband’s/partner’s education (higher levels of education correlate with lower rates of abuse) are linked to higher levels of abuse. 33 These data represent gender, social and behavioural norms that contribute to a woman’s inability to advocate for protecting herself, including for safe sex, increasing her risk for HIV infection. Social, Cultural and Gender Norms A patriarchal society in Zimbabwe inhibits women’s ability to contribute equally to society and relationships, leaving them disempowered in terms of safer sex, health decision-making and financial stability. Employment among adult women ages 25-49 is 55% to 65%, lower than that among men (89% to 92%), which limits their authority and decision-making capabilities. 33 Studies also found that in sub-Saharan Africa women lack autonomy to make decisions about HIV testing and services. 48 In Zimbabwe, women describe the fear of domestic violence and divorce for accessing HIV services without consent from their husband. If a woman tests positive for HIV, her husband might blame and abuse her for bringing HIV into their relationship. Serodiscordant Relationships In Zimbabwe, 9% of couples are in a serodiscordant relationship, where the man is HIV positive and the woman is HIV negative, 33 and more than a third (38%) of new infections are among people in stable relationships. 48 Couples counselling and HIV testing have been shown to reduce heterosexually transmitted HIV infections that would otherwise occur, but uptake for couples counselling tends to be low. 49
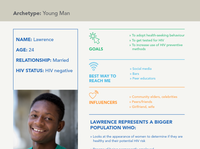
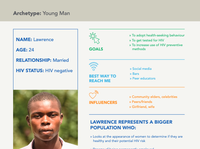
3. 66 COMPREHENSIVE NATIONAL HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 “I know my husband has girlfriends. How long can I stay HIV negative when I don’t know my husband’s status?” Archetype: Adult Woman » Friends » Spouse, sister and mother » Health workers » Social networks » Radio » Health workers Abbreviations: PrEP, pre-exposure prophylaxis. » To seek family planning services and get tested for HIV » To initiate PrEP » For her husband to get tested for HIV NAME: Shamiso AGE: 35 RELATIONSHIP: Married but doesn’t know her husband’s status HIV STATUS: HIV negative GOALS BEST WAY TO REACH ME INFLUENCERS SHAMISO REPRESENTS A BIGGER POPULATION WHO: » Values family, church, friends and social status » Thinks being healthy means living a long and healthy life – being there for her children as they grow up » Spends most of her time at work and at home » Gets information from radio, internet, SMS (Econet) and women’s groups; she trusts information on health from radio and health workers » Doesn’t trust talking to her friends and other relatives about health » Gets information from church/prophets and traditional healers » Is motivated to stay healthy for her children » Believes her husband’s friends are a negative influence on his health and HIV prevention » Thinks HIV self-testing could make testing easier for her husband Adult Woman Health Journey Map: Shamiso, 35 years old, HIV negative About this map: This is a theoretical high-level health journey for an adult woman interacting with HIV and SRH programmes, which may overlap or be sequential. The journey map reveals her experience and what she might be doing, thinking and feeling along the way that impact her desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Hospitals, health facility, TV, Dreams programme, NGOs that teach people about health, church; Other sources: radio, friends, family, traditional/faith leaders, village health workers, internet, SMS messages (Econet) Integration of HIV with Family Planning Services: Having two children already, she is concerned about being able to afford more. She is interested in a family planning method. This is an entry point to HIV testing and an opportunity for her to understand her risks. She wants her and her husband to know each other’s status. Programmes should take advantage of opportunities to integrate HIV testing with family planning services Increase Awareness of PrEP: She is concerned about the stigma associated with taking PrEP; she does not want people/husband to think that she is taking ARVs for HIV. Misinformation and lack of access to information about PrEP can impede adoption of this effective HIV prevention method. She would like to have the most up-to-date information, so she can feel confident. When she starts PrEP, she hides the pills so her husband won’t find them Couples Counselling and Testing: Uptake for HIV testing is low among men. Therefore, HIV testing and counselling supports mutual disclosure and empowers couples to make informed decisions together about HIV prevention and reproductive health. Awareness campaigns and radio dramas about couples testing are a way to decrease stigma and normalise testing among those in committed relationships
5. 68 COMPREHENSIVE NATIONAL HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Communications Matrix: Adult Women DESIRED CHANGES* TO SEEK FAMILY PLANNING TO PREVENT UNPLANNED PREGNANCY AND GET TESTED FOR HIV TO ACCESS HIV PREVENTION METHODS, SPECIFICALLY PREP TO GET PARTNER TESTED FOR HIV Barriers • Cost and distance to health facility • Health worker attitude - lack of respect • Religious beliefs and practices • Gender norms • Fear of disclosure of HIV test and negative or positive result • Lack of awareness and knowledge of PrEP • Providers see her as high-risk • Self-stigma, fear or denial • Myths and misconceptions about PrEP • Fear that being seen taking pills equates to being HIV positive • Fear of side effects and negative attitude of health workers • Cost and distance of medication refill • He believes he is not at risk, so he doesn’t want to get tested • HIV stigma and gender-based violence • Cost and distance and time to seek services • Fear of disclosure and fear of losing the relationship Facilitating Factors • Quality, friendly and respectful services • Privacy and confidentiality • Supportive spouse • Reduced/affordable costs • Positive peer influence • Use of ambassadors/champions • Staying healthy • Living longer • Supportive family, partner, community • Testimonials from satisfied peers • Reduced cost and distance to health facilities • Couples counselling and testing • Influence from traditional healers, religious leaders and community elders Communications Objectives 1. Increase positive community perceptions of women accessing family planning 2. Increase positive provider attitudes and perceptions about women accessing health services 3. Increase knowledge, awareness, attitudes and perceptions of PrEP among at-risk populations and providers 4. Increase positive community perceptions about couples counselling and testing
4. 67 Adult Woman Health Journey Map: Shamiso, 35 years old, HIV negative About this map: This is a theoretical high-level health journey for an adult woman interacting with HIV and SRH programmes, which may overlap or be sequential. The journey map reveals her experience and what she might be doing, thinking and feeling along the way that impact her desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Hospitals, health facility, TV, Dreams programme, NGOs that teach people about health, church; Other sources: radio, friends, family, traditional/faith leaders, village health workers, internet, SMS messages (Econet) Integration of HIV with Family Planning Services: Having two children already, she is concerned about being able to afford more. She is interested in a family planning method. This is an entry point to HIV testing and an opportunity for her to understand her risks. She wants her and her husband to know each other’s status. Programmes should take advantage of opportunities to integrate HIV testing with family planning services Increase Awareness of PrEP: She is concerned about the stigma associated with taking PrEP; she does not want people/husband to think that she is taking ARVs for HIV. Misinformation and lack of access to information about PrEP can impede adoption of this effective HIV prevention method. She would like to have the most up-to-date information, so she can feel confident. When she starts PrEP, she hides the pills so her husband won’t find them Couples Counselling and Testing: Uptake for HIV testing is low among men. Therefore, HIV testing and counselling supports mutual disclosure and empowers couples to make informed decisions together about HIV prevention and reproductive health. Awareness campaigns and radio dramas about couples testing are a way to decrease stigma and normalise testing among those in committed relationships Positive emotion Neutral emotion Negative emotion Shamiso’s Experience Key Insights Doing: Sees the health care worker about family planning Thinking: I do not want to get pregnant. I know my husband has many girlfriends Feeling: Optimistic, Stable Doing: Hears about PrEP; reads brochure Thinking: Maybe PrEP could be good for me Feeling: Informed, Optimistic Doing: Talks to health care provider about family planning options and HIV testing Thinking: I should probably get tested; I do not know my husband’s status Feeling: Determined, Proactive Doing: Talks to the health worker about PrEP, but they have very little information Thinking: Who else can I talk to about PrEP? Feeling: Confused, Conflicted, Frustrated Doing: Gets tested; receives HIV-negative result. Starts family planning method Thinking: I am so glad it is negative; I want to continue to protect myself Feeling: Empowered, Relieved Doing: Goes to an HIV clinic to begin PrEP Thinking: I am so relieved that I can protect myself Feeling: Empowered, Happy Doing: Hears a radio drama about partner testing with her husband Thinking: I hope that he is paying attention to the radio programme Feeling: Hopeful, Optimistic Doing: Talks to her husband about getting HIV tested; he agrees Thinking: I am so glad we heard that radio drama, it made it easier to talk about HIV testing Feeling: Relieved Family Planning and HIV Testing Services Prevention: PrEP HIV Testing Services: Partner Testing Abbreviations: ARV, antiretroviral; NGO, nongovernmental organisation; PrEP, pre-exposure prophylaxis; SRH, sexual and reproductive health.