2. 71 Table 10. Adolescent Boys and Young Men: Synopsis of Problem and Desired Behaviours and Practices PROBLEM BEHAVIOURS/PRACTICES DESIRED BEHAVIOURS/PRACTICES • Limited knowledge about HIV and prevention methods • Inconsistent and incorrect condom use; low risk perception for themselves and that of women they have sex with • Risky sexual behaviours: multiple sex partners, sex with sex workers • Fear of using a condom incorrectly in front of partner • Low rates of HIV testing • Does not disclose status to sex partners; fear in disclosing HIV-positive results to partner or family; lack of access to age-appropriate counselling on partner disclosure • Does not seek health services; lack of empowerment related to interactions with providers • Socio-cultural and religious beliefs and doctrines leading to perceptions of masculinity; “hyper- masculine” attitudes and behaviours (multiple sex partners, domestic violence, etc.) in an effort to assert their manhood • Practice safe sex and reduce risky behaviours such as multiple partners, sex with sex workers, inconsistent condom use • Improve knowledge, attitudes and perceptions of HIV prevention (HIV testing/self-testing, condoms and PrEP), treatment and care • Seek and use HIV prevention (self-testing, male and female condoms, and PrEP), care and treatment • Engage with male mobilisers and community- based health care providers as a bridge to the health care system • Providers to deliver empathetic, client-centred, male-friendly and confidential care • Disclose HIV testing and status to partner
1. 70 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Adolescent Boys and Young Men ABYM: Situation and Behavioural Analysis HIV prevalence among adolescent boys (15-19 years) and young men (20-24 years) tends to be low (2.5% and 2.7%, respectively), but the rate steadily climbs until it peaks at 28.1% among men ages 45-49 years. 7 Almost a third of boys (30%) have had sex before the age of 18 years, but HIV testing coverage is low at 35%. 39 Inadequate and limited access or inability to read comprehensive HIV prevention, care and treatment information, along with myths and misconceptions, contribute to ABYM’s risk of HIV infection. ABYM are shy to talk about sex, which limits their ability to acquire information about HIV prevention, care and treatment. A man’s need to feel in control underpins his behaviour (see adult men sub-strategy for more information). When seeking HIV prevention, care and treatment, ABYM feel less in control because of a lack of knowledge and fear about the process of an HIV test and pain associated with the needle prick, preventing uptake of services. Additionally, fears of an HIV-positive result, partner disclosure, and losing a relationship compound the anxiety around HIV testing. Moreover, ABYM worry about how they are seen in the community, including the implications such as not being able to work or have a healthy family one day. Regarding condoms, ABYM worry about the shame and embarrassment of how to access them at shops, taking free ones from the clinic, partner perception of condom quality and how to use them properly. Furthermore, ABYM fear being seen at the clinic and worry about health care workers disclosing his status to his friends and family, which further inhibits HIV prevention, care and treatment service uptake. Peer Influence, Mutual Support and Social Proof Peers have a high level of influence (positive and negative) about SRH and HIV information and behaviour. They are driven by the opinions and actions of their peers; social proof and peer acceptance can influence their decisions towards doing things together. Mutual support reduces the fear of shame and regret because they are all doing it together. 41 Moreover, for those who have not had sex yet, anticipated sexual debut can provide motivation to get circumcised because of perceptions about sexual benefits. Cultural and religious norms including those enforced by traditional healers, pastors and elders can negatively influence ABYM (and people in general) in seeking HIV prevention, care and treatment if the services fall outside the doctrine or their beliefs. Religious leaders who preach abstinence often fail to believe that people in their congregation engage in behaviours that predispose them to HIV infection. Anecdotally, men report gauging HIV risk based on appearance and familiarity and assume the HIV status of his partner if her results are HIV negative.
6. 75 * For simplicity, all content within this matrix matches the HIV status and journey of the archetype. However, a desired change along with matching illustrative messages have been identified for the alternative HIV status. Abbreviations: ART, antiretroviral therapy; HTS, HIV testing services; PrEP, pre-exposure prophylaxis, SRH, sexual and reproductive health; STI, sexually transmitted infections; VMMC, voluntary medical male circumcision. Illustrative Messages • HIV testing is available in my community—my friend and I got tested Messages for Parents: • It is in the best interest of your child to get him or her tested for HIV • Teach your children to take responsibility for their health encourage them to get an HIV test • First time in the game? Play by the rules, wear a condom • My friend got circumcised, I can do it too • I got circumcised because it is the smart thing to do—now my friends are circumcised too • More and more people are getting circumcised in the community including famous people like and MPs • There is pain but it is manageable; you can get help with the pain using pain medicine and there are tips for how to reduce pain • You should expect pain on injection, during erections, day 2, and upon bandage removal • I’m circumcised, I condomise, my game is safe Illustrative Messages for desired change for HIV positive Adolescent Boy: To get initiated on ART and stay virally suppressed* • I have accepted my HIV positive result, despite how I got it, and I am starting my treatment today • I adhere to my treatment—I feel great • My loved ones know my status—I have all the support I need • I will never stop my HIV treatment—my life depends on it • Life goes on for people with HIV—I am a living proof • My friend is HIV negative; I am HIV positive, but we both have bright futur es ahead of us! Illustrative Indicators 1. % of target audience with accurate knowledge of HIV and adolescent sexual and reproductive health services 2. % of target audience expressing accepting attitudes to adolescent boys accessing HIV and sexual reproductive health services 3. % of adolescent boys who report high self-efficacy for accessing HIV and sexual and reproductive health services 4. % of adolescent boys who report increased HIV health risk perception 5. # of people reached with age-appropriate messages on importance of HIV and sexual and reproductive services for adolescent boys 6. % of adolescent boys who agree that condoms provide effective protection against (a) STIs and (b) HIV 7. % of adolescent boys who report that they know how to use condoms consistently and correctly 8. % of adolescent boys who report that they know where to access condoms 9. Number of adolescent boys exposed to age-appropriate messages on HIV and sexual and reproductive health services for adolescents 10. Number of providers trained on client-centred care for adolescents 11. Number of community dialogue meetings held to sensitise communities on the importance of HIV and sexual r eproductive health services for adolescents
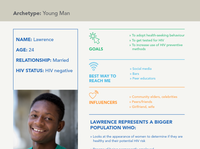
3. 72 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 “Will it hurt me? Will leave a scar? What if I get an erection while the wound is healing?” Archetype: Adolescent Boy » Anyone with high social status » Friends » Uncle, father, older brother » Social hangouts » Peer networks » Social media Abbreviations: VMMC, voluntary medical male circumcision. » To get tested for HIV » To use condoms consistently and correctly » To get circumcised NAME: James AGE: 16 RELATIONSHIP: Has a girlfriend HIV STATUS: HIV negative GOALS BEST WAY TO REACH ME INFLUENCERS JAMES REPRESENTS A BIGGER POPULATION WHO: » Is motivated by social proof and driven by the opinions and actions of their peers » Feels shy buying or taking free condoms, making it difficult for them to use them consistently and correctly » Is influenced by aspirational needs to mimic high social status individuals such as drug dealers or gangsters » Thinks group support provides them a mutual support mechanism and reduces fear of shame and regret » Feels their anticipated sexual debut can be seen as a motivation to get circumcised » Is most receptive to communication via social media » Wants peer educators to talk to them where they are – at the pool hall, and other local hang outs » Has difficulty accessing HIV services because of poverty, stigma, not being able to comprehend the HIV information » Feels confidentiality, privacy and security is important Adolescent Boy Health Journey Map: James, 16 years old, HIV negative About this map: This is a theoretical high-level health journey for an adolescent boy interacting with three HIV programmes, which may overlap or be sequential. The journey map reveals his experience and what he might be doing, thinking and feeling along the way that could impact his desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Teachers, parents, providers, digital media, peer networks, radio programmes, posters and billboards, community health workers, celebrities/football players/musicians with lived experience; Other sources: Radio music programmes, TV, posters and billboards, community health workers Social and Cultural Norms: Social and cultural norms make it difficult for him to talk about sexual and reproductive health. He fears being tested for HIV because of past behaviours (e.g. unprotected sex) that have put him at risk. He worries that if he is HIV positive he will have HIV-positive children and that he won’t be able to work to support his family. He worries that his status would be leaked by health workers Social Proof/Peer Influence: Social acceptance is important to him; he worries about being made fun of by his peers if he admi ts not knowing how to use a condom. He gets most of his information from school teachers/counsellors, friends or health workers. He needs information on how to use condoms correctly. He wishes his parents received health information about his needs so that they could understand him better Feeling of Control: He is most worried about the pain of VMMC and the risks associated with the procedure. It can take two years or more to adopt VMMC from awareness to completing the procedure. It takes time, and feeling in control is the most important thing to him. Generally, he would like additional health information, not limited to VMMC
4. 73 Adolescent Boy Health Journey Map: James, 16 years old, HIV negative About this map: This is a theoretical high-level health journey for an adolescent boy interacting with three HIV programmes, which may overlap or be sequential. The journey map reveals his experience and what he might be doing, thinking and feeling along the way that could impact his desire and ability to access services The red, dark red and gray dots indicate the highs/positive emotion (motivators) and lows/negative emotion (barriers) of the journey. These help the reader of the map prioritise opportunities for communications interventions and collaboration with service delivery to make the journey easier Trusted information sources: Teachers, parents, providers, digital media, peer networks, radio programmes, posters and billboards, community health workers, celebrities/football players/musicians with lived experience; Other sources: Radio music programmes, TV, posters and billboards, community health workers Social and Cultural Norms: Social and cultural norms make it difficult for him to talk about sexual and reproductive health. He fears being tested for HIV because of past behaviours (e.g. unprotected sex) that have put him at risk. He worries that if he is HIV positive he will have HIV-positive children and that he won’t be able to work to support his family. He worries that his status would be leaked by health workers Social Proof/Peer Influence: Social acceptance is important to him; he worries about being made fun of by his peers if he admi ts not knowing how to use a condom. He gets most of his information from school teachers/counsellors, friends or health workers. He needs information on how to use condoms correctly. He wishes his parents received health information about his needs so that they could understand him better Feeling of Control: He is most worried about the pain of VMMC and the risks associated with the procedure. It can take two years or more to adopt VMMC from awareness to completing the procedure. It takes time, and feeling in control is the most important thing to him. Generally, he would like additional health information, not limited to VMMC Positive emotion Neutral emotion Negative emotion James’ Experience Key Insights Doing: Goes to school. Spends time with his friends, playing sports and hanging out with his girlfriend Thinking: Why would I need to get tested for HIV? The girls I’ve had sex with looked healthy Feeling: Indifferent, Ambivalent, Not worried Doing: Gets free condoms from the health worker; talks to his friends and girlfriend about using condoms Thinking: I wonder if sex will feel good using a condom; I wonder what my girlfriend will say Feeling: Neutral, Ambivalent, Curious Doing: Talks about HIV testing with a health worker who visits his school Thinking: Maybe I should get tested for HIV to be sure I do not have it Feeling: Nervous, Anxious Doing: Uses condom with his girlfriend, but he didn’t know how to use it and it breaks Thinking: I do not understand why it broke; I wish I knew how to use it properly Feeling: Frustrated, Embarrassed, Angry, Defeated Doing: Goes for testing at the youth center health clinic; talks to the health worker about testing and condoms. Gets tested and is HIV negative Thinking: If I test to be HIV negative I will never do anything risky like have unprotected sex ever again Feeling: Relieved, Happy, Optimistic Doing: Talks to a peer educator at the pool hall Thinking: I have been hearing people talk about VMMC, but I have heard it is painful Feeling: Curious, Interested Doing: Talks to his older brother and uncle about VMMC. Asks them if they are circumcised Thinking: If I were to do the procedure, would it be painful? Maybe it is worth the pain because it can protect from HIV transmission Feeling: Unsure, Curious, Fearful Doing: Reads brochures about VMMC; talks to friends at school about it; asks them if they are circumcised Thinking: Maybe I would do the procedure if some of my friends do it too Feeling: Unsure, Ambivalent, Informed HIV Testing Services Prevention: Condoms Prevention: VMMC Abbreviations: SRH, sexual and reproductive health; VMMC, voluntary medical male circumcision.
5. 74 COMPREHENSIVE HIV COMMUNICATIONS STRATEGY FOR ZIMBABWE: 2019-2025 Communications Matrix: Adolescent Boys DESIRED CHANGES* TO GET TESTED FOR HIV TO GET AND USE CONDOMS CONSISTENTLY AND CORRECTLY TO GET CIRCUMCISED Barriers • Lack of comprehensive information on HIV and SRH • Low perceived risk • Peer pressure • Fear of positive result • Lack of privacy and confidentiality at the local health facility • Stigma and discrimination • Age of consent • Attitude of service provider • User fees for SRH services • Stigma associated with accessing condoms • Lack of knowledge on how to correctly use the condom • Peer pressure not to use condoms • Lack of access to condoms • Misperceptions about condom brands and quality • Lack of variety in public-sector condoms • Social and cultural norms preventing parents/ guardians conversations with adolescents about sexual and reproductive health • Fear of pain • Lack of peer support • Myths and misconceptions especially on foreskin disposal • Lack of parental support for consenting to procedure • Accessibility of services • Lack of age-appropriate communications approaches and information on SRH, HIV and VMMC Facilitating Factors • Peer support • Availability of information on the benefits of HTS and STI prevention • Availability of adolescent-friendly services and provider • HIV Self Testing • Adolescent-friendly services • Peer support • Increased self-efficiency on how to use condoms • Access to condom varieties • Peer and social support • Availability of services • Knowledge of HIV and SRH Communications Objectives 1. Increase knowledge, attitudes and perceptions on access and benefits of HIV and SRH services 2. Reduce stigma and discrimination from family and community members 3. Increase self-efficacy to access HIV services 4. Increase risk perception of HIV 5. Improve attitudes and perceived value of condom use by adolescents 6. Increase knowledge on how to use condoms consistently and correctly 7. Increase knowledge of and improve attitudes and perceptions of where to access condoms 8. Improve age-appropriate knowledge of VMMC 9. Increase positive community attitudes and perceptions on access to VMMC services Illustrative Messages • Know your HIV status, seek testing and protect yourself • I overcame my fears and went for HIV testing • My peers are getting tested for HIV—so should I • I am my own man—I went for an HIV test • Make informed decisions—use condoms correctly and consistently • Cool guys do not compromise—they condomise • All condoms are safe and effective—use one condom each time • My future is bright—I condomise • Protect yourself and get circumcised • I am cool and smart—I am circumcised • I am in control of my health—I got circumcised • You may experience some pain after VMMC, but it is manageable. You will not be bed-ridden